Abstract
Parkinson’s disease (PD) is a prevalent neurodegenerative disorder traditionally defined by its motor symptoms yet increasingly recognized for its wide spectrum of neuropsychiatric symptoms (NPS) including anxiety, depression, apathy, impulse-control behaviors, and hallucinations. Recent neuroimaging advances have provided crucial insights into the neural substrates underlying these comorbidities. Structural imaging studies, using voxel-based morphometry and T1-weighted magnetic resonance imaging, have revealed regional atrophy in the frontal cortex, striatum, limbic areas, and occipital regions. In comparison, functional imaging using positron emission tomography, single-photon emission computed tomography, and resting-state functional MRI have identified abnormal network connectivity in circuits implicated in fear processing, reward regulation, and cognitive control. Overall, these imaging studies suggest shared and distinct pathophysiology of PD-related NPS, emphasizing the need for longitudinal, multimodal investigations to inform targeted therapeutic strategies and to improve clinical outcomes.
Introduction
Parkinson's disease (PD) is one of the most common neurodegenerative disorders worldwide, clinically defined by the presence of bradykinesia with at least one additional cardinal motor feature—rigidity or resting tremor—with a host of supportive and exclusionary criteria[1-2] . Globally, PD affects approximately 0.3% of the population, with a mean onset in the early 50s; however, onset may occur as early as before age 40 and as late as in the 80s[3] . Incidence increases markedly with age, reaching about 1% in individuals over 65 and up to 3% in those older than 80[4] . With rising life expectancy, the number of PD cases and their associated socioeconomic burdens are projected to increase dramatically[2] . Furthermore, the incidence, prevalence, and mortality risk of PD is higher in men than in women by a ratio of approximately 1.4:1[2] . Early-onset PD—typically defined as onset before 45 years—is often associated with a genetic etiology, accounting for roughly 10% of cases, and up to 40% in those with onset before 30 years[5-6] .
While the motor features of PD remain its diagnostic cornerstone, non-motor symptoms are increasingly recognized as critical components of the disease and may even precede motor signs by several years. Non-motor signs include neuropsychiatric symptoms, disturbances in sleep–wake regulation, cognitive deficits (such as executive dysfunction, memory retrieval problems, dementia, and hallucinations), autonomic dysfunction (including orthostatic hypotension, urogenital disturbances, constipation, and hyperhidrosis), sensory deficits (most notably olfactory impairment), and pain[7] . These symptoms can significantly affect quality of life, overall disability, and need for long-term care[3] .
Neuropsychiatric Symptoms in Parkinson's Disease
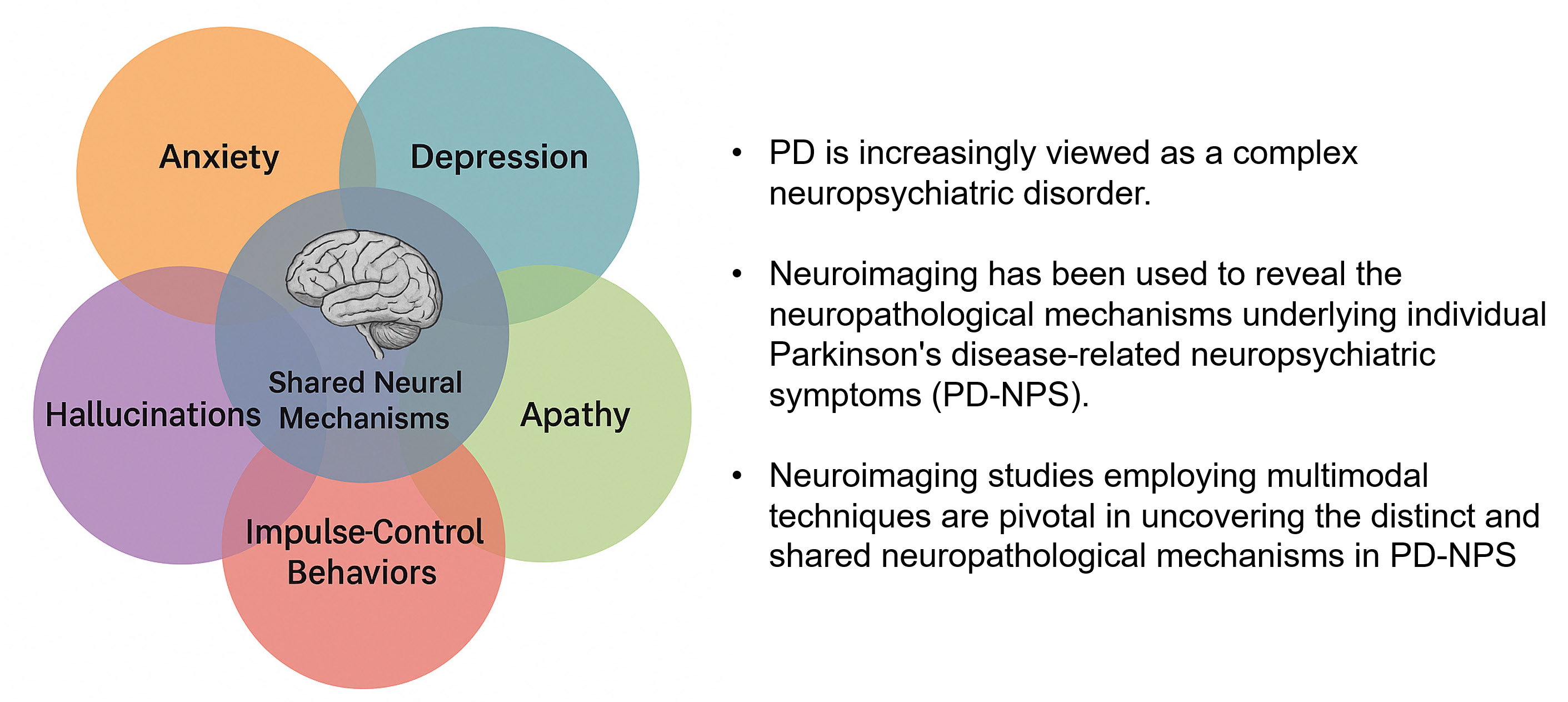
PD is increasingly viewed as a complex neuropsychiatric disorder. Neuropsychiatric symptoms (NPS) in PD can be broadly classified into three domains: affective (e.g., depression and anxiety), perceptual or cognitive (e.g., hallucinations), and motivational (e.g., impulse-compulsive behaviors (ICBs) and apathy)[8-9] . Approximately 56% of early, untreated PD patients experience one or more neuropsychiatric disturbances[10] . Although patients may initially present with a single NPS, the progression of PD is frequently marked by an exacerbation and overlap of NPS, complicating both diagnosis and management[11-12] .
In patients with early-stage PD, depression and anxiety are the most common NPS. Depression often emerges in the early stages of the disease, with its prevalence increasing as age and disease duration. In advanced-stage PD patients, up to 60% exhibit comorbid depressive symptoms[13] . Approximately 30-35% of PD patients may experience significant anxiety symptoms[14] . Mild hallucinations, particularly non-visual hallucinations, frequently occur in early PD[15] . Studies report that 25-40% of PD patients may experience mild psychosis, while around 4% develop delusions[16] . As the disease progresses, the prevalence of remission in late-stage PD can reach 60%[17-18] . Compared to other NPS, apathy has received relatively less research attention, with an average prevalence of approximately 35-40%[19-20] . ICBs encompass impulse control disorders (pathological gambling, compulsive shopping, hypersexuality, and binge eating), dopamine dysregulation syndrome (compulsive use of anti-PD medications), and stereotyped behaviors (repetitive, non-goal-directed activities). Among patients receiving dopaminergic therapy, the prevalence of impulse control disorders is approximately 15%[21] , with the incidence increasing over the course of the disease[22] ; the cumulative incidence over five years reaches 46%[23] . Dopamine dysregulation syndrome and stereotyped behaviors often overlap with impulse control disorders and are predominantly observed in patients taking high doses of levodopa[8] .
NPS in PD are heterogeneous, and debate persists over whether NPS in PD result from PD pathology or from nonspecific effects of psychosocial deterioration and secondary, psychological sequelae[8] . Epidemiological data reveal that PD patients exhibit distinct hallucinations and ICBs compared to general psychiatric conditions, suggesting a PD-specific pathophysiology. However, it remains uncertain if PD-related anxiety and depression differ from those in primary psychiatric disorders or in the general population[8,24-25] . Early-stage NPS, particularly depression and anxiety, may arise from psychosocial factors, whereas later-stage symptoms are more associated with PD pathology and dopaminergic treatment exposure[8] . Longitudinal studies have identified risk factors for NPS such as age, gender, disease severity, and dopaminergic therapy, with over 50% of PD patients developing three or more NPS within five years[26-28] .
Although NPS significantly impair the quality of life in patients with PD, clinical research on their treatment lags far behind advancements in managing motor symptoms. Given the complex interplay between motor and non-motor symptoms, their high comorbidity, and the potential that treating one symptom will impact others, effective management requires clinical expertise and interdisciplinary collaboration[29-30] . Dopamine therapy in PD patients may exacerbate psychosis[29-30] and ICBs[31] while improving apathy[32-33] . Non-dopamine treatment strategies primarily encompass pharmacotherapy and psychotherapy. Research has demonstrated the safety and efficacy of several antidepressants in PD patients, including selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants, with comparable efficacy across these drug classes[34] . Pimavanserin has shown promising efficacy and tolerability in treating psychosis, with randomized controlled trials currently underway. Glutamatergic antagonist amantadine may improve apathy[35] and ICBs[31-36] . Psychological interventions, such as cognitive behavioral therapy (CBT), have been shown to ameliorate depressive symptoms in PD patients[37-38] . Other therapeutic approaches, including bilateral deep brain stimulation (DBS) of the medial globus pallidus or subthalamic nucleus, repetitive transcranial magnetic stimulation (rTMS), electroconvulsive therapy, light therapy, and aerobic exercise, are also generating considerable interest[39-42] .
Utilizing neuroimaging to study the neuropathological mechanisms PD-NPS can help identify region-specific atrophy, dysfunctional network connectivity, and neurotransmitter abnormalities through multimodal techniques (structural MRI, fMRI, PET/SPECT). These insights uncover heterogeneous pathological substrates that clinical assessments alone cannot detect. By bridging gaps in behavioral research, neuroimaging enables targeted therapeutic development, intervention optimization, and disease trajectory prediction. Ultimately, neuroimaging can better inform precision medicine for PD-NPS. The following sections review recent imaging studies that have advanced our understanding of the neural substrates underlying anxiety, depression, apathy, ICBs and hallucinations in PD.
Neuroimaging Studies on Anxiety
Anxiety is among the most common non-motor symptoms in PD, with an estimated prevalence of 31%—higher than observed in the general population or in patients with other medical conditions[14] . Despite anxiety’s clinical impact and association with reduced quality of life[43-45] , its neural mechanisms in PD remain incompletely understood.
Neuroimaging has implicated two major neural circuits in anxiety pathogenesis within PD patients. The first is the fear circuit involving the amygdala, anterior cingulate cortex (ACC), medial prefrontal cortex (mPFC), insular cortex, hippocampus, and striatum[46] . The second circuit is the limbic-cortico-striatal-thalamocortical network connecting the prefrontal cortex (PFC), basal ganglia, and thalamus[47-46] . In PD, degeneration of dopaminergic, noradrenergic, and serotonergic neurons within these circuits likely contributes to the high prevalence of anxiety[48] .
Voxel-based morphometry (VBM) studies have demonstrated that higher anxiety scores—assessed using instruments such as the Beck Anxiety Inventory[49] —are associated with reduced gray matter volumes in the bilateral ACC, left amygdala, precuneus, and cerebellar structures[50-52] . Structural covariance analyses indicate that anxiety severity inversely correlates with the connectivity integrity between the striatum and prefrontal regions[53] . Functional MRI (fMRI) investigations have revealed aberrant low-frequency oscillatory activity in the right cerebellum and orbital frontal cortex (OFC) among PD patients with anxiety[54] . In addition, enhanced functional connectivity between the amygdala and OFC, as well as between parietal and medial temporal cortices, has been documented, suggesting that anomalous network interactions and anxiety symptoms are linked[55-57] . Neurotransmitter imaging with positron emission tomography (PET) and single-photon emission computed tomography (SPECT) further support these findings; decreased binding of dopamine transporters (DAT) in the caudate, thalamus, insula, ACC, and PCC is associated with increased anxiety[58-61] .
Neuroimaging Studies on Depression
Depression in PD has been extensively studied using metabolic imaging techniques such as PET and SPECT. Most investigations report hypometabolism in the frontal and striatal regions in depressed PD patients, as compared to both non-depressed PD cohorts and healthy controls[62] . Abnormal metabolic patterns have been identified in the prefrontal cortex, thalamus, amygdala, hippocampus, ACC, insula, and raphe nuclei[62,61] . In contrast, a few studies have observed hypermetabolism in subcortical structures (e.g., the caudate, putamen, and amygdala) with a positive correlation to depressive symptom severity[63-64] . Dysregulated activity in the amygdala has also been observed in depressed PD patients[63-65] . Moreover, both FDG-PET and H₂¹⁵O PET studies consistently report reduced metabolism in the OFC of these patients[66-67] .
Structural MRI studies using T1-weighted imaging have consistently demonstrated atrophy in the PFC, parietal, thalamus and limbic regions (notably the ACC, hippocampus and amygdala) in PD patients with depression[62,68-69] . Several studies emphasize marked atrophy in the OFC and ACC—regions pivotal for cognitive control and emotional regulation[70-73] . Diffusion tensor imaging (DTI) studies reveal decreased white matter integrity in tracts connecting the ACC, thalamus, and frontotemporal regions[74-76] . In addition, resting-state fMRI studies have shown that depressed PD patients exhibit both increased and decreased intrinsic activity across various networks, reflecting disrupted connectivity within cortico-limbic circuits[65,77-78] . Collectively, these imaging findings suggest that depression in PD arises from the dysregulation of frontal–limbic circuits and is compounded by abnormalities in dopaminergic, serotonergic, and noradrenergic neurotransmission[62] .
Neuroimaging Studies on Apathy
Apathy is a common non-motor symptom in PD, defined as a lack of motivation that is not attributable to diminished consciousness, cognitive impairment, or emotional distress. Structural MRI studies indicate that apathy in PD is associated with cortical thinning and atrophy in the temporal lobe, frontal cortex, parietal regions, ACC and hippocampus; key subcortical structures such as the putamen, caudate nucleus and accumbens are also affected[79-82] . Resting-state fMRI studies revealing reduced functional connectivity between the striatum and frontal regions have implicated disruptions in cortico–subcortical limbic networks in apathy pathophysiology[83-84] . Metabolic imaging studies generally report negative correlations between apathy and regional metabolism in the striatum, cerebellum, and various cortical areas; however, in some instances, increased metabolism in the OFC and ACC may represent compensatory responses[85-86] . Further, PET studies have demonstrated that severe dopaminergic denervation—especially within the mesolimbic pathway—is associated with greater apathy, especially following deep brain stimulation[87-88] . While serotonergic and cholinergic dysfunctions have also been implicated[89] , the current evidence supports a multifactorial etiology of apathy in PD.
Neuroimaging Studies on Impulse-Control Behaviors
ICDs in PD, which include pathological gambling, hypersexuality, compulsive eating, and compulsive shopping, are frequently associated with long-term dopaminergic therapy[90] . The core clinical features of ICDs are repetitive, compulsive behaviors that are initially rewarding but progressively difficult to control[23] . Recent imaging studies suggest that ICDs may result from a combination of dopaminergic treatment and underlying vulnerability in reward-processing circuits.
Structural MRI findings in PD patients with ICDs are mixed. Some studies report cortical thinning in the frontal cortex and reduced volumes in the nucleus accumbens and OFC[91-92] ; other studies find increased cortical thickness in frontal and cingulate regions, potentially reflecting neuroplastic changes related to excessive dopaminergic stimulation[93-94] . Further, functional MRI studies reveal an association between ICDs and disrupted connectivity within dopaminergic networks, notably between the striatum, prefrontal cortex, and limbic areas[95-97] . Task-based fMRI studies employing reward-based paradigms have consistently shown altered activation in the OFC and caudate nucleus; this evidence supports the hypothesis that impaired reward processing contributes to ICD development[95,98-99] . Importantly, imaging studies in drug-naïve PD patients suggest that pre-existing network abnormalities in mesolimbic and executive circuits may predispose individuals to ICDs upon initiation of dopaminergic therapy[100-101] .
Neuroimaging Studies on Hallucinations
Hallucinations in PD typically begin with minor phenomena—such as brief passage hallucinations, illusions, or the sense of a presence. However, they may evolve to be more visually complex, particularly in advanced stages of the disease. Patients often retain insight initially; however, as the disease progresses, insight diminishes while delusional thinking and multimodal hallucinations emerge[15,102] .
In PD patients with visual hallucinations, structural imaging studies consistently report atrophy in occipital regions—most notably within the lateral and ventral occipitotemporal cortices[103-104] . Some investigations controlling for cognitive status also document atrophy in frontal, hippocampal, and thalamic regions[105-106] . Although white matter studies are relatively sparse, recent evidence points to reductions in occipital and parahippocampal white matter volume in patients with psychosis[107-109] . Functional imaging studies during hallucinatory episodes are rare. Available data indicate that reduced occipital region activity, combined with aberrant frontal activation, may underlie the emergence of visual hallucinations[110-111] . Furthermore, altered connectivity among occipital, frontal, striatal, and thalamic regions—and increased co-activation of default mode network nodes—appears to contribute to psychosis vulnerability in PD[112] .
Neuroimaging Studies of Multiple Neuropsychiatric Symptoms
It is not uncommon for PD patients to experience a combination of anxiety, depression, and apathy—a constellation often described as the “non-motor triad” of PD[113] . Neuroimaging studies have revealed that the severity of these overlapping symptoms is linked to the degree of dopaminergic and noradrenergic denervation in key limbic regions such as the ACC, thalamus, amygdala, and ventral striatum[114] . Although several neurotransmitter imaging studies report overlapping mechanisms, others delineate distinct neural signatures for individual symptoms. For example, while anxiety and depression both correlate with diminished dopaminergic activity in the ventral striatum, specific patterns of connectivity—such as differential involvement of the caudate nucleus versus other striatal subregions—may distinguish these conditions[55,57,115] . Moreover, the frequent co-occurrence of depression and ICDs in PD suggests that shared disturbances in ventral striatal dopaminergic transmission, and associated cortico-striatal-limbic circuits, may underlie both disorders[116] . These overlapping yet distinct imaging findings underscore the complexity of neuropsychiatric manifestations in PD and highlight the need for integrative, multimodal imaging approaches.
A recent study reported that five neuropsychiatric symptoms in PD exhibit coordinated effects on brain morphometric profiles. Apathy, ICBs, and hallucinations share structural abnormalities in the somatomotor and visual areas. In contrast, the cortical abnormalities associated with anxiety and depression were most prominent in the prefrontal cortex and default mode network regions. These findings indicate that distinct mechanisms underlie different NPS: apathy, ICBs, and hallucinations may be directly linked to the primary neuropathology of PD within motor circuits, whereas anxiety and depression—whose neurobiological bases are less clearly defined—may arise from a combination of PD-related pathology (e.g., a hypodopaminergic state) and psychological factors[117] .
Conclusions
Neuroimaging studies employing multimodal techniques are pivotal in uncovering the distinct and shared neuropathological mechanisms of Parkinson’s disease-related neuropsychiatric symptoms. These studies collectively advance therapeutic precision and mechanistic understanding through revealing region-specific atrophy, disrupted functional connectivity, and neurotransmitter dysregulation. Despite these advances, current research is often constrained by small sample sizes, cross-sectional designs, and a focus on individual symptoms rather than a broader spectrum of neuropsychiatric manifestations. Future research should prioritize larger-scale, longitudinal, and multimodal imaging studies to further elucidate the complex neural networks involved. A more comprehensive understanding of these mechanisms is essential to advance targeted therapies, enhance clinical management, and ultimately improve patient outcomes in PD.
<Acknowledgements
Not applicable.
Author contributions
Ethics approval and consent to participate
Not applicable.
Funding information
Not applicable.
Competing Interests
The authors declare that they have no existing or potential commercial or financial relationships that could create a conflict of interest at the time of conducting this study.
Data Availability
All data needed to evaluate the conclusions in the paper are present in the paper or the Supplementary Materials. Additional data related to this paper may be requested from the authors.
References
[1] Tolosa E, Garrido A, Scholz SW, Poewe W. Challenges in the diagnosis of Parkinson's disease. Lancet Neurol 2021;20:385-397.
[2] Ben-Shlomo Y, Darweesh S, Llibre-Guerra J, Marras C, San Luciano M, Tanner C. The epidemiology of Parkinson's disease. Lancet 2024;403:283-292.
[3] Poewe W, Seppi K, Tanner CM, et al. Parkinson disease. Nat Rev Dis Primers 2017;3:17013.
[4] Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson's disease: a systematic review and meta-analysis. Mov Disord 2014;29:1583-1590.
[5] Alcalay RN, Caccappolo E, Mejia-Santana H, et al. Frequency of known mutations in early-onset Parkinson disease: implication for genetic counseling: the consortium on risk for early onset Parkinson disease study. Arch Neurol 2010;67:1116-1122.
[6] Marder KS, Tang MX, Mejia-Santana H, et al. Predictors of parkin mutations in early-onset Parkinson disease: the consortium on risk for early-onset Parkinson disease study. Arch Neurol 2010;67:731-738.
[7] Chaudhuri KR, Schapira AH. Non-motor symptoms of Parkinson's disease: dopaminergic pathophysiology and treatment. Lancet Neurol 2009;8:464-474.
[8] Weintraub D, Aarsland D, Chaudhuri KR, et al. The neuropsychiatry of Parkinson's disease: advances and challenges. Lancet Neurol 2022;21:89-102.
[9] Costello H, Schrag AE, Howard R, Roiser JP. Dissociable effects of dopaminergic medications on depression symptom dimensions in Parkinson disease. Nat Ment Health 2024;2:916-923.
[10] Aarsland D, Bronnick K, Alves G, et al. The spectrum of neuropsychiatric symptoms in patients with early untreated Parkinson's disease. J Neurol Neurosurg Psychiatry 2009;80:928-930.
[11] Kim R, Shin JH, Park S, Kim HJ, Jeon B. Longitudinal evolution of non-motor symptoms according to age at onset in early Parkinson's disease. J Neurol Sci 2020;418:117157.
[12] Ou R, Lin J, Liu K, et al. Evolution of Apathy in Early Parkinson's Disease: A 4-Years Prospective Cohort Study. Front Aging Neurosci 2020;12:620762.
[13] Yamamoto H. [Immunoglobulins in periapical lesion with special reference to qualitative and quantitative analysis of IgG]. Tsurumi Shigaku 1989;15:27-47.
[14] Broen MP, Narayen NE, Kuijf ML, Dissanayaka NN, Leentjens AF. Prevalence of anxiety in Parkinson's disease: A systematic review and meta-analysis. Mov Disord 2016;31:1125-1133.
[15] Pagonabarraga J, Martinez-Horta S, Fernandez de Bobadilla R, et al. Minor hallucinations occur in drug-naive Parkinson's disease patients, even from the premotor phase. Mov Disord 2016;31:45-52.
[16] Fenelon G, Soulas T, Zenasni F, Cleret de Langavant L. The changing face of Parkinson's disease-associated psychosis: a cross-sectional study based on the new NINDS-NIMH criteria. Mov Disord 2010;25:763-766.
[17] Dlay JK, Duncan GW, Khoo TK, et al. Progression of Neuropsychiatric Symptoms over Time in an Incident Parkinson's Disease Cohort (ICICLE-PD). Brain Sci 2020;10.
[18] Barrell K, Bureau B, Turcano P, et al. High-Order Visual Processing, Visual Symptoms, and Visual Hallucinations: A Possible Symptomatic Progression of Parkinson's Disease. Front Neurol 2018;9:999.
[19] Santangelo G, Trojano L, Barone P, Errico D, Grossi D, Vitale C. Apathy in Parkinson's disease: diagnosis, neuropsychological correlates, pathophysiology and treatment. Behav Neurol 2013;27:501-513.
[20] den Brok MG, van Dalen JW, van Gool WA, Moll van Charante EP, de Bie RM, Richard E. Apathy in Parkinson's disease: A systematic review and meta-analysis. Mov Disord 2015;30:759-769.
[21] Weintraub D, Koester J, Potenza MN, et al. Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol 2010;67:589-595.
[22] Markovic V, Stankovic I, Petrovic I, et al. Dynamics of impulsive-compulsive behaviors in early Parkinson's disease: a prospective study. J Neurol 2020;267:1127-1136.
[23] Corvol JC, Artaud F, Cormier-Dequaire F, et al. Longitudinal analysis of impulse control disorders in Parkinson disease. Neurology 2018;91:e189-e201.
[24] Gustafsson H, Nordstrom A, Nordstrom P. Depression and subsequent risk of Parkinson disease: A nationwide cohort study. Neurology 2015;84:2422-2429.
[25] Kazmi H, Walker Z, Booij J, et al. Late onset depression: dopaminergic deficit and clinical features of prodromal Parkinson's disease: a cross-sectional study. J Neurol Neurosurg Psychiatry 2021;92:158-164.
[26] Marinus J, Zhu K, Marras C, Aarsland D, van Hilten JJ. Risk factors for non-motor symptoms in Parkinson's disease. Lancet Neurol 2018;17:559-568.
[27] Hommel A, Meinders MJ, Lorenzl S, et al. The Prevalence and Determinants of Neuropsychiatric Symptoms in Late-Stage Parkinsonism. Mov Disord Clin Pract 2020;7:531-542.
[28] Weintraub D, Caspell-Garcia C, Simuni T, et al. Neuropsychiatric symptoms and cognitive abilities over the initial quinquennium of Parkinson disease. Ann Clin Transl Neurol 2020;7:449-461.
[29] Mueller C, Rajkumar AP, Wan YM, et al. Assessment and Management of Neuropsychiatric Symptoms in Parkinson's Disease. CNS Drugs 2018;32:621-635.
[30] Aarsland D, Marsh L, Schrag A. Neuropsychiatric symptoms in Parkinson's disease. Mov Disord 2009;24:2175-2186.
[31] Mamikonyan E, Siderowf AD, Duda JE, et al. Long-term follow-up of impulse control disorders in Parkinson's disease. Mov Disord 2008;23:75-80.
[32] Czernecki V, Pillon B, Houeto JL, Pochon JB, Levy R, Dubois B. Motivation, reward, and Parkinson's disease: influence of dopatherapy. Neuropsychologia 2002;40:2257-2267.
[33] Leentjens AF, Koester J, Fruh B, Shephard DT, Barone P, Houben JJ. The effect of pramipexole on mood and motivational symptoms in Parkinson's disease: a meta-analysis of placebo-controlled studies. Clin Ther 2009;31:89-98.
[34] Mills KA, Greene MC, Dezube R, Goodson C, Karmarkar T, Pontone GM. Efficacy and tolerability of antidepressants in Parkinson's disease: A systematic review and network meta-analysis. Int J Geriatr Psychiatry 2018;33:642-651.
[35] Kaji Y, Hirata K. Apathy and anhedonia in Parkinson's disease. ISRN Neurol 2011;2011:219427.
[36] Thomas A, Bonanni L, Gambi F, Di Iorio A, Onofrj M. Pathological gambling in Parkinson disease is reduced by amantadine. Ann Neurol 2010;68:400-404.
[37] Dobkin RD, Mann SL, Gara MA, Interian A, Rodriguez KM, Menza M. Telephone-based cognitive behavioral therapy for depression in Parkinson disease: A randomized controlled trial. Neurology 2020;94:e1764-e1773.
[38] Dobkin RD, Mann SL, Weintraub D, et al. Innovating Parkinson's Care: A Randomized Controlled Trial of Telemedicine Depression Treatment. Mov Disord 2021;36:2549-2558.
[39] Seppi K, Ray Chaudhuri K, Coelho M, et al. Update on treatments for nonmotor symptoms of Parkinson's disease-an evidence-based medicine review. Mov Disord 2019;34:180-198.
[40] Li S, Jiao R, Zhou X, Chen S. Motor recovery and antidepressant effects of repetitive transcranial magnetic stimulation on Parkinson disease: A PRISMA-compliant meta-analysis. Medicine (Baltimore) 2020;99:e19642.
[41] Lin F, Su Y, Weng Y, et al. The effects of bright light therapy on depression and sleep disturbances in patients with Parkinson's disease: a systematic review and meta-analysis of randomized controlled trials. Sleep Med 2021;83:280-289.
[42] Wu PL, Lee M, Huang TT. Effectiveness of physical activity on patients with depression and Parkinson's disease: A systematic review. PLoS One 2017;12:e0181515.
[43] Pontone GM, Williams JR, Anderson KE, et al. Anxiety and self-perceived health status in Parkinson's disease. Parkinsonism Relat Disord 2011;17:249-254.
[44] Leentjens AF, Dujardin K, Marsh L, Martinez-Martin P, Richard IH, Starkstein SE. Symptomatology and markers of anxiety disorders in Parkinson's disease: a cross-sectional study. Mov Disord 2011;26:484-492.
[45] Leentjens AF, Dujardin K, Marsh L, Martinez-Martin P, Richard IH, Starkstein SE. Anxiety and motor fluctuations in Parkinson's disease: a cross-sectional observational study. Parkinsonism Relat Disord 2012;18:1084-1088.
[46] Carey G, Gormezoglu M, de Jong JJA, et al. Neuroimaging of Anxiety in Parkinson's Disease: A Systematic Review. Mov Disord 2021;36:327-339.
[47] Volkmann J, Daniels C, Witt K. Neuropsychiatric effects of subthalamic neurostimulation in Parkinson disease. Nat Rev Neurol 2010;6:487-498.
[48] Thobois S, Prange S, Sgambato-Faure V, Tremblay L, Broussolle E. Imaging the Etiology of Apathy, Anxiety, and Depression in Parkinson's Disease: Implication for Treatment. Curr Neurol Neurosci Rep 2017;17:76.
[49] Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893-897.
[50] Vriend C, Boedhoe PS, Rutten S, Berendse HW, van der Werf YD, van den Heuvel OA. A smaller amygdala is associated with anxiety in Parkinson's disease: a combined FreeSurfer-VBM study. J Neurol Neurosurg Psychiatry 2016;87:493-500.
[51] Wee N, Wen MC, Kandiah N, et al. Neural correlates of anxiety symptoms in mild Parkinson's disease: A prospective longitudinal voxel-based morphometry study. J Neurol Sci 2016;371:131-136.
[52] Ma X, Su W, Li S, et al. Cerebellar atrophy in different subtypes of Parkinson's disease. J Neurol Sci 2018;392:105-112.
[53] Oosterwijk CS, Vriend C, Berendse HW, van der Werf YD, van den Heuvel OA. Anxiety in Parkinson's disease is associated with reduced structural covariance of the striatum. J Affect Disord 2018;240:113-120.
[54] Wang X, Li J, Wang M, et al. Alterations of the amplitude of low-frequency fluctuations in anxiety in Parkinson's disease. Neurosci Lett 2018;668:19-23.
[55] Zhang H, Qiu Y, Luo Y, et al. The relationship of anxious and depressive symptoms in Parkinson's disease with voxel-based neuroanatomical and functional connectivity measures. J Affect Disord 2019;245:580-588.
[56] Wang X, Li J, Yuan Y, et al. Altered putamen functional connectivity is associated with anxiety disorder in Parkinson's disease. Oncotarget 2017;8:81377-81386.
[57] Dan R, Ruzicka F, Bezdicek O, et al. Separate neural representations of depression, anxiety and apathy in Parkinson's disease. Sci Rep 2017;7:12164.
[58] Picillo M, Santangelo G, Erro R, et al. Association between dopaminergic dysfunction and anxiety in de novo Parkinson's disease. Parkinsonism Relat Disord 2017;37:106-110.
[59] Joling M, van den Heuvel OA, Berendse HW, Booij J, Vriend C. Serotonin transporter binding and anxiety symptoms in Parkinson's disease. J Neurol Neurosurg Psychiatry 2018;89:89-94.
[60] Bayram E, Kaplan N, Shan G, Caldwell JZK. The longitudinal associations between cognition, mood and striatal dopaminergic binding in Parkinson's Disease. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn 2020;27:581-594.
[61] Maillet A, Metereau E, Tremblay L, et al. Serotonergic and Dopaminergic Lesions Underlying Parkinsonian Neuropsychiatric Signs. Mov Disord 2021;36:2888-2900.
[62] Wen MC, Chan LL, Tan LC, Tan EK. Depression, anxiety, and apathy in Parkinson's disease: insights from neuroimaging studies. Eur J Neurol 2016;23:1001-1019.
[63] Huang C, Ravdin LD, Nirenberg MJ, et al. Neuroimaging markers of motor and nonmotor features of Parkinson's disease: an 18f fluorodeoxyglucose positron emission computed tomography study. Dement Geriatr Cogn Disord 2013;35:183-196.
[64] Ceravolo R, Frosini D, Poletti M, et al. Mild affective symptoms in de novo Parkinson's disease patients: relationship with dopaminergic dysfunction. Eur J Neurol 2013;20:480-485.
[65] Huang P, Xuan M, Gu Q, et al. Abnormal amygdala function in Parkinson's disease patients and its relationship to depression. J Affect Disord 2015;183:263-268.
[66] Mayberg HS, Starkstein SE, Sadzot B, et al. Selective hypometabolism in the inferior frontal lobe in depressed patients with Parkinson's disease. Ann Neurol 1990;28:57-64.
[67] Mentis MJ, McIntosh AR, Perrine K, et al. Relationships among the metabolic patterns that correlate with mnemonic, visuospatial, and mood symptoms in Parkinson's disease. Am J Psychiatry 2002;159:746-754.
[68] Badenoch JB, Paris A, Jacobs BM, Noyce AJ, Marshall CR, Waters S. Neuroanatomical and prognostic associations of depression in Parkinson's disease. J Neurol Neurosurg Psychiatry 2024;95:966-973.
[69] Yuan J, Liu Y, Liao H, et al. Alterations in cortical volume and complexity in Parkinson's disease with depression. CNS Neurosci Ther 2024;30:e14582.
[70] Feldmann A, Illes Z, Kosztolanyi P, et al. Morphometric changes of gray matter in Parkinson's disease with depression: a voxel-based morphometry study. Mov Disord 2008;23:42-46.
[71] Kostic VS, Agosta F, Petrovic I, et al. Regional patterns of brain tissue loss associated with depression in Parkinson disease. Neurology 2010;75:857-863.
[72] Deng X, Tang CY, Zhang J, et al. The cortical thickness correlates of clinical manifestations in the mid-stage sporadic Parkinson's disease. Neurosci Lett 2016;633:279-289.
[73] Surdhar I, Gee M, Bouchard T, Coupland N, Malykhin N, Camicioli R. Intact limbic-prefrontal connections and reduced amygdala volumes in Parkinson's disease with mild depressive symptoms. Parkinsonism Relat Disord 2012;18:809-813.
[74] Huang P, Xu X, Gu Q, et al. Disrupted white matter integrity in depressed versus non-depressed Parkinson's disease patients: a tract-based spatial statistics study. J Neurol Sci 2014;346:145-148.
[75] Li W, Liu J, Skidmore F, Liu Y, Tian J, Li K. White matter microstructure changes in the thalamus in Parkinson disease with depression: A diffusion tensor MR imaging study. AJNR Am J Neuroradiol 2010;31:1861-1866.
[76] Salehi MA, Mohammadi S, Gouravani M, Javidi A, Dager SR. Brain microstructural alterations of depression in Parkinson's disease: A systematic review of diffusion tensor imaging studies. Hum Brain Mapp 2022;43:5658-5680.
[77] Hu X, Song X, Yuan Y, et al. Abnormal functional connectivity of the amygdala is associated with depression in Parkinson's disease. Mov Disord 2015;30:238-244.
[78] Lou Y, Huang P, Li D, et al. Altered brain network centrality in depressed Parkinson's disease patients. Mov Disord 2015;30:1777-1784.
[79] Carriere N, Besson P, Dujardin K, et al. Apathy in Parkinson's disease is associated with nucleus accumbens atrophy: a magnetic resonance imaging shape analysis. Mov Disord 2014;29:897-903.
[80] Alzahrani H, Antonini A, Venneri A. Apathy in Mild Parkinson's Disease: Neuropsychological and Neuroimaging Evidence. J Parkinsons Dis 2016;6:821-832.
[81] Theis H, Prange S, Bischof GN, et al. Impulsive-compulsive behaviour in early Parkinson's disease is determined by apathy and dopamine receptor D3 polymorphism. NPJ Parkinsons Dis 2023;9:154.
[82] Ge S, Liu J, Jia Y, Li Z, Wang J, Wang M. Topological alteration of the brain structural network in Parkinson's disease with apathy. Brain Res Bull 2024;208:110899.
[83] Baggio HC, Segura B, Garrido-Millan JL, et al. Resting-state frontostriatal functional connectivity in Parkinson's disease-related apathy. Mov Disord 2015;30:671-679.
[84] Lucas-Jimenez O, Ojeda N, Pena J, et al. Apathy and brain alterations in Parkinson's disease: a multimodal imaging study. Ann Clin Transl Neurol 2018;5:803-814.
[85] Robert G, Le Jeune F, Lozachmeur C, et al. Apathy in patients with Parkinson disease without dementia or depression: a PET study. Neurology 2012;79:1155-1160.
[86] Robert GH, Le Jeune F, Lozachmeur C, et al. Preoperative factors of apathy in subthalamic stimulated Parkinson disease: a PET study. Neurology 2014;83:1620-1626.
[87] Zoon TJC, Mathiopoulou V, van Rooijen G, et al. Apathy following deep brain stimulation in Parkinson's disease visualized by 7-Tesla MRI subthalamic network analysis. Brain Stimul 2023;16:1289-1291.
[88] Boon LI, Potters WV, Zoon TJC, et al. Structural and functional correlates of subthalamic deep brain stimulation-induced apathy in Parkinson's disease. Brain Stimul 2021;14:192-201.
[89] Prange S, Metereau E, Maillet A, et al. Limbic Serotonergic Plasticity Contributes to the Compensation of Apathy in Early Parkinson's Disease. Mov Disord 2022;37:1211-1221.
[90] Voon V, Napier TC, Frank MJ, et al. Impulse control disorders and levodopa-induced dyskinesias in Parkinson's disease: an update. Lancet Neurol 2017;16:238-250.
[91] Biundo R, Weis L, Facchini S, et al. Patterns of cortical thickness associated with impulse control disorders in Parkinson's disease. Mov Disord 2015;30:688-695.
[92] Cerasa A, Salsone M, Nigro S, et al. Cortical volume and folding abnormalities in Parkinson's disease patients with pathological gambling. Parkinsonism Relat Disord 2014;20:1209-1214.
[93] Pellicano C, Niccolini F, Wu K, et al. Morphometric changes in the reward system of Parkinson's disease patients with impulse control disorders. J Neurol 2015;262:2653-2661.
[94] Tessitore A, Santangelo G, De Micco R, et al. Cortical thickness changes in patients with Parkinson's disease and impulse control disorders. Parkinsonism Relat Disord 2016;24:119-125.
[95] Petersen K, Van Wouwe N, Stark A, et al. Ventral striatal network connectivity reflects reward learning and behavior in patients with Parkinson's disease. Hum Brain Mapp 2018;39:509-521.
[96] Carriere N, Lopes R, Defebvre L, Delmaire C, Dujardin K. Impaired corticostriatal connectivity in impulse control disorders in Parkinson disease. Neurology 2015;84:2116-2123.
[97] Maggi G, Loayza F, Vitale C, Santangelo G, Obeso I. Anatomical correlates of apathy and impulsivity co-occurrence in early Parkinson's disease. J Neurol 2024;271:2798-2809.
[98] Gescheidt T, Marecek R, Mikl M, et al. Functional anatomy of outcome evaluation during Iowa Gambling Task performance in patients with Parkinson's disease: an fMRI study. Neurol Sci 2013;34:2159-2166.
[99] Frosini D, Pesaresi I, Cosottini M, et al. Parkinson's disease and pathological gambling: results from a functional MRI study. Mov Disord 2010;25:2449-2453.
[100] van der Vegt JP, Hulme OJ, Zittel S, et al. Attenuated neural response to gamble outcomes in drug-naive patients with Parkinson's disease. Brain 2013;136:1192-1203.
[101] Tessitore A, De Micco R, Giordano A, et al. Intrinsic brain connectivity predicts impulse control disorders in patients with Parkinson's disease. Mov Disord 2017;32:1710-1719.
[102] Fenelon G, Alves G. Epidemiology of psychosis in Parkinson's disease. J Neurol Sci 2010;289:12-17.
[103] Carter R, Ffytche DH. On visual hallucinations and cortical networks: a trans-diagnostic review. J Neurol 2015;262:1780-1790.
[104] Lenka A, Jhunjhunwala KR, Saini J, Pal PK. Structural and functional neuroimaging in patients with Parkinson's disease and visual hallucinations: A critical review. Parkinsonism Relat Disord 2015;21:683-691.
[105] Ozawa M, Shiraishi T, Murakami H, et al. Structural MRI study of Pareidolia and Visual Hallucinations in Drug-Naive Parkinson's disease. Sci Rep 2024;14:31293.
[106] Bhome R, Thomas GEC, Zarkali A, Weil RS. Structural and Functional Imaging Correlates of Visual Hallucinations in Parkinson's Disease. Curr Neurol Neurosci Rep 2023;23:287-299.
[107] Watanabe H, Senda J, Kato S, et al. Cortical and subcortical brain atrophy in Parkinson's disease with visual hallucination. Mov Disord 2013;28:1732-1736.
[108] Pezzoli S, Cagnin A, Bandmann O, Venneri A. Structural and Functional Neuroimaging of Visual Hallucinations in Lewy Body Disease: A Systematic Literature Review. Brain Sci 2017;7.
[109] Yao N, Cheung C, Pang S, et al. Multimodal MRI of the hippocampus in Parkinson's disease with visual hallucinations. Brain Struct Funct 2016;221:287-300.
[110] Goetz CG, Vaughan CL, Goldman JG, Stebbins GT. I finally see what you see: Parkinson's disease visual hallucinations captured with functional neuroimaging. Mov Disord 2014;29:115-117.
[111] Yao N, Pang S, Cheung C, et al. Resting activity in visual and corticostriatal pathways in Parkinson's disease with hallucinations. Parkinsonism Relat Disord 2015;21:131-137.
[112] Yao N, Shek-Kwan Chang R, Cheung C, et al. The default mode network is disrupted in Parkinson's disease with visual hallucinations. Hum Brain Mapp 2014;35:5658-5666.
[113] Maillet A, Krack P, Lhommee E, et al. The prominent role of serotonergic degeneration in apathy, anxiety and depression in de novo Parkinson's disease. Brain 2016;139:2486-2502.
[114] Remy P, Doder M, Lees A, Turjanski N, Brooks D. Depression in Parkinson's disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain 2005;128:1314-1322.
[115] Prange S, Metereau E, Maillet A, et al. Early limbic microstructural alterations in apathy and depression in de novo Parkinson's disease. Mov Disord 2019;34:1644-1654.
[116] Vriend C, Pattij T, van der Werf YD, et al. Depression and impulse control disorders in Parkinson's disease: two sides of the same coin? Neurosci Biobehav Rev 2014;38:60-71.
[117] Lu Q, Zhu Z, Zhang H, et al. Shared and distinct cortical morphometric alterations in five neuropsychiatric symptoms of Parkinson's disease. Transl Psychiatry 2024;14:347.
 Figures
Figures References
References Peer
Peer Information
Information[1] Tolosa E, Garrido A, Scholz SW, Poewe W. Challenges in the diagnosis of Parkinson's disease. Lancet Neurol 2021;20:385-397.
[2] Ben-Shlomo Y, Darweesh S, Llibre-Guerra J, Marras C, San Luciano M, Tanner C. The epidemiology of Parkinson's disease. Lancet 2024;403:283-292.
[3] Poewe W, Seppi K, Tanner CM, et al. Parkinson disease. Nat Rev Dis Primers 2017;3:17013.
[4] Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson's disease: a systematic review and meta-analysis. Mov Disord 2014;29:1583-1590.
[5] Alcalay RN, Caccappolo E, Mejia-Santana H, et al. Frequency of known mutations in early-onset Parkinson disease: implication for genetic counseling: the consortium on risk for early onset Parkinson disease study. Arch Neurol 2010;67:1116-1122.
[6] Marder KS, Tang MX, Mejia-Santana H, et al. Predictors of parkin mutations in early-onset Parkinson disease: the consortium on risk for early-onset Parkinson disease study. Arch Neurol 2010;67:731-738.
[7] Chaudhuri KR, Schapira AH. Non-motor symptoms of Parkinson's disease: dopaminergic pathophysiology and treatment. Lancet Neurol 2009;8:464-474.
[8] Weintraub D, Aarsland D, Chaudhuri KR, et al. The neuropsychiatry of Parkinson's disease: advances and challenges. Lancet Neurol 2022;21:89-102.
[9] Costello H, Schrag AE, Howard R, Roiser JP. Dissociable effects of dopaminergic medications on depression symptom dimensions in Parkinson disease. Nat Ment Health 2024;2:916-923.
[10] Aarsland D, Bronnick K, Alves G, et al. The spectrum of neuropsychiatric symptoms in patients with early untreated Parkinson's disease. J Neurol Neurosurg Psychiatry 2009;80:928-930.
[11] Kim R, Shin JH, Park S, Kim HJ, Jeon B. Longitudinal evolution of non-motor symptoms according to age at onset in early Parkinson's disease. J Neurol Sci 2020;418:117157.
[12] Ou R, Lin J, Liu K, et al. Evolution of Apathy in Early Parkinson's Disease: A 4-Years Prospective Cohort Study. Front Aging Neurosci 2020;12:620762.
[13] Yamamoto H. [Immunoglobulins in periapical lesion with special reference to qualitative and quantitative analysis of IgG]. Tsurumi Shigaku 1989;15:27-47.
[14] Broen MP, Narayen NE, Kuijf ML, Dissanayaka NN, Leentjens AF. Prevalence of anxiety in Parkinson's disease: A systematic review and meta-analysis. Mov Disord 2016;31:1125-1133.
[15] Pagonabarraga J, Martinez-Horta S, Fernandez de Bobadilla R, et al. Minor hallucinations occur in drug-naive Parkinson's disease patients, even from the premotor phase. Mov Disord 2016;31:45-52.
[16] Fenelon G, Soulas T, Zenasni F, Cleret de Langavant L. The changing face of Parkinson's disease-associated psychosis: a cross-sectional study based on the new NINDS-NIMH criteria. Mov Disord 2010;25:763-766.
[17] Dlay JK, Duncan GW, Khoo TK, et al. Progression of Neuropsychiatric Symptoms over Time in an Incident Parkinson's Disease Cohort (ICICLE-PD). Brain Sci 2020;10.
[18] Barrell K, Bureau B, Turcano P, et al. High-Order Visual Processing, Visual Symptoms, and Visual Hallucinations: A Possible Symptomatic Progression of Parkinson's Disease. Front Neurol 2018;9:999.
[19] Santangelo G, Trojano L, Barone P, Errico D, Grossi D, Vitale C. Apathy in Parkinson's disease: diagnosis, neuropsychological correlates, pathophysiology and treatment. Behav Neurol 2013;27:501-513.
[20] den Brok MG, van Dalen JW, van Gool WA, Moll van Charante EP, de Bie RM, Richard E. Apathy in Parkinson's disease: A systematic review and meta-analysis. Mov Disord 2015;30:759-769.
[21] Weintraub D, Koester J, Potenza MN, et al. Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol 2010;67:589-595.
[22] Markovic V, Stankovic I, Petrovic I, et al. Dynamics of impulsive-compulsive behaviors in early Parkinson's disease: a prospective study. J Neurol 2020;267:1127-1136.
[23] Corvol JC, Artaud F, Cormier-Dequaire F, et al. Longitudinal analysis of impulse control disorders in Parkinson disease. Neurology 2018;91:e189-e201.
[24] Gustafsson H, Nordstrom A, Nordstrom P. Depression and subsequent risk of Parkinson disease: A nationwide cohort study. Neurology 2015;84:2422-2429.
[25] Kazmi H, Walker Z, Booij J, et al. Late onset depression: dopaminergic deficit and clinical features of prodromal Parkinson's disease: a cross-sectional study. J Neurol Neurosurg Psychiatry 2021;92:158-164.
[26] Marinus J, Zhu K, Marras C, Aarsland D, van Hilten JJ. Risk factors for non-motor symptoms in Parkinson's disease. Lancet Neurol 2018;17:559-568.
[27] Hommel A, Meinders MJ, Lorenzl S, et al. The Prevalence and Determinants of Neuropsychiatric Symptoms in Late-Stage Parkinsonism. Mov Disord Clin Pract 2020;7:531-542.
[28] Weintraub D, Caspell-Garcia C, Simuni T, et al. Neuropsychiatric symptoms and cognitive abilities over the initial quinquennium of Parkinson disease. Ann Clin Transl Neurol 2020;7:449-461.
[29] Mueller C, Rajkumar AP, Wan YM, et al. Assessment and Management of Neuropsychiatric Symptoms in Parkinson's Disease. CNS Drugs 2018;32:621-635.
[30] Aarsland D, Marsh L, Schrag A. Neuropsychiatric symptoms in Parkinson's disease. Mov Disord 2009;24:2175-2186.
[31] Mamikonyan E, Siderowf AD, Duda JE, et al. Long-term follow-up of impulse control disorders in Parkinson's disease. Mov Disord 2008;23:75-80.
[32] Czernecki V, Pillon B, Houeto JL, Pochon JB, Levy R, Dubois B. Motivation, reward, and Parkinson's disease: influence of dopatherapy. Neuropsychologia 2002;40:2257-2267.
[33] Leentjens AF, Koester J, Fruh B, Shephard DT, Barone P, Houben JJ. The effect of pramipexole on mood and motivational symptoms in Parkinson's disease: a meta-analysis of placebo-controlled studies. Clin Ther 2009;31:89-98.
[34] Mills KA, Greene MC, Dezube R, Goodson C, Karmarkar T, Pontone GM. Efficacy and tolerability of antidepressants in Parkinson's disease: A systematic review and network meta-analysis. Int J Geriatr Psychiatry 2018;33:642-651.
[35] Kaji Y, Hirata K. Apathy and anhedonia in Parkinson's disease. ISRN Neurol 2011;2011:219427.
[36] Thomas A, Bonanni L, Gambi F, Di Iorio A, Onofrj M. Pathological gambling in Parkinson disease is reduced by amantadine. Ann Neurol 2010;68:400-404.
[37] Dobkin RD, Mann SL, Gara MA, Interian A, Rodriguez KM, Menza M. Telephone-based cognitive behavioral therapy for depression in Parkinson disease: A randomized controlled trial. Neurology 2020;94:e1764-e1773.
[38] Dobkin RD, Mann SL, Weintraub D, et al. Innovating Parkinson's Care: A Randomized Controlled Trial of Telemedicine Depression Treatment. Mov Disord 2021;36:2549-2558.
[39] Seppi K, Ray Chaudhuri K, Coelho M, et al. Update on treatments for nonmotor symptoms of Parkinson's disease-an evidence-based medicine review. Mov Disord 2019;34:180-198.
[40] Li S, Jiao R, Zhou X, Chen S. Motor recovery and antidepressant effects of repetitive transcranial magnetic stimulation on Parkinson disease: A PRISMA-compliant meta-analysis. Medicine (Baltimore) 2020;99:e19642.
[41] Lin F, Su Y, Weng Y, et al. The effects of bright light therapy on depression and sleep disturbances in patients with Parkinson's disease: a systematic review and meta-analysis of randomized controlled trials. Sleep Med 2021;83:280-289.
[42] Wu PL, Lee M, Huang TT. Effectiveness of physical activity on patients with depression and Parkinson's disease: A systematic review. PLoS One 2017;12:e0181515.
[43] Pontone GM, Williams JR, Anderson KE, et al. Anxiety and self-perceived health status in Parkinson's disease. Parkinsonism Relat Disord 2011;17:249-254.
[44] Leentjens AF, Dujardin K, Marsh L, Martinez-Martin P, Richard IH, Starkstein SE. Symptomatology and markers of anxiety disorders in Parkinson's disease: a cross-sectional study. Mov Disord 2011;26:484-492.
[45] Leentjens AF, Dujardin K, Marsh L, Martinez-Martin P, Richard IH, Starkstein SE. Anxiety and motor fluctuations in Parkinson's disease: a cross-sectional observational study. Parkinsonism Relat Disord 2012;18:1084-1088.
[46] Carey G, Gormezoglu M, de Jong JJA, et al. Neuroimaging of Anxiety in Parkinson's Disease: A Systematic Review. Mov Disord 2021;36:327-339.
[47] Volkmann J, Daniels C, Witt K. Neuropsychiatric effects of subthalamic neurostimulation in Parkinson disease. Nat Rev Neurol 2010;6:487-498.
[48] Thobois S, Prange S, Sgambato-Faure V, Tremblay L, Broussolle E. Imaging the Etiology of Apathy, Anxiety, and Depression in Parkinson's Disease: Implication for Treatment. Curr Neurol Neurosci Rep 2017;17:76.
[49] Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893-897.
[50] Vriend C, Boedhoe PS, Rutten S, Berendse HW, van der Werf YD, van den Heuvel OA. A smaller amygdala is associated with anxiety in Parkinson's disease: a combined FreeSurfer-VBM study. J Neurol Neurosurg Psychiatry 2016;87:493-500.
[51] Wee N, Wen MC, Kandiah N, et al. Neural correlates of anxiety symptoms in mild Parkinson's disease: A prospective longitudinal voxel-based morphometry study. J Neurol Sci 2016;371:131-136.
[52] Ma X, Su W, Li S, et al. Cerebellar atrophy in different subtypes of Parkinson's disease. J Neurol Sci 2018;392:105-112.
[53] Oosterwijk CS, Vriend C, Berendse HW, van der Werf YD, van den Heuvel OA. Anxiety in Parkinson's disease is associated with reduced structural covariance of the striatum. J Affect Disord 2018;240:113-120.
[54] Wang X, Li J, Wang M, et al. Alterations of the amplitude of low-frequency fluctuations in anxiety in Parkinson's disease. Neurosci Lett 2018;668:19-23.
[55] Zhang H, Qiu Y, Luo Y, et al. The relationship of anxious and depressive symptoms in Parkinson's disease with voxel-based neuroanatomical and functional connectivity measures. J Affect Disord 2019;245:580-588.
[56] Wang X, Li J, Yuan Y, et al. Altered putamen functional connectivity is associated with anxiety disorder in Parkinson's disease. Oncotarget 2017;8:81377-81386.
[57] Dan R, Ruzicka F, Bezdicek O, et al. Separate neural representations of depression, anxiety and apathy in Parkinson's disease. Sci Rep 2017;7:12164.
[58] Picillo M, Santangelo G, Erro R, et al. Association between dopaminergic dysfunction and anxiety in de novo Parkinson's disease. Parkinsonism Relat Disord 2017;37:106-110.
[59] Joling M, van den Heuvel OA, Berendse HW, Booij J, Vriend C. Serotonin transporter binding and anxiety symptoms in Parkinson's disease. J Neurol Neurosurg Psychiatry 2018;89:89-94.
[60] Bayram E, Kaplan N, Shan G, Caldwell JZK. The longitudinal associations between cognition, mood and striatal dopaminergic binding in Parkinson's Disease. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn 2020;27:581-594.
[61] Maillet A, Metereau E, Tremblay L, et al. Serotonergic and Dopaminergic Lesions Underlying Parkinsonian Neuropsychiatric Signs. Mov Disord 2021;36:2888-2900.
[62] Wen MC, Chan LL, Tan LC, Tan EK. Depression, anxiety, and apathy in Parkinson's disease: insights from neuroimaging studies. Eur J Neurol 2016;23:1001-1019.
[63] Huang C, Ravdin LD, Nirenberg MJ, et al. Neuroimaging markers of motor and nonmotor features of Parkinson's disease: an 18f fluorodeoxyglucose positron emission computed tomography study. Dement Geriatr Cogn Disord 2013;35:183-196.
[64] Ceravolo R, Frosini D, Poletti M, et al. Mild affective symptoms in de novo Parkinson's disease patients: relationship with dopaminergic dysfunction. Eur J Neurol 2013;20:480-485.
[65] Huang P, Xuan M, Gu Q, et al. Abnormal amygdala function in Parkinson's disease patients and its relationship to depression. J Affect Disord 2015;183:263-268.
[66] Mayberg HS, Starkstein SE, Sadzot B, et al. Selective hypometabolism in the inferior frontal lobe in depressed patients with Parkinson's disease. Ann Neurol 1990;28:57-64.
[67] Mentis MJ, McIntosh AR, Perrine K, et al. Relationships among the metabolic patterns that correlate with mnemonic, visuospatial, and mood symptoms in Parkinson's disease. Am J Psychiatry 2002;159:746-754.
[68] Badenoch JB, Paris A, Jacobs BM, Noyce AJ, Marshall CR, Waters S. Neuroanatomical and prognostic associations of depression in Parkinson's disease. J Neurol Neurosurg Psychiatry 2024;95:966-973.
[69] Yuan J, Liu Y, Liao H, et al. Alterations in cortical volume and complexity in Parkinson's disease with depression. CNS Neurosci Ther 2024;30:e14582.
[70] Feldmann A, Illes Z, Kosztolanyi P, et al. Morphometric changes of gray matter in Parkinson's disease with depression: a voxel-based morphometry study. Mov Disord 2008;23:42-46.
[71] Kostic VS, Agosta F, Petrovic I, et al. Regional patterns of brain tissue loss associated with depression in Parkinson disease. Neurology 2010;75:857-863.
[72] Deng X, Tang CY, Zhang J, et al. The cortical thickness correlates of clinical manifestations in the mid-stage sporadic Parkinson's disease. Neurosci Lett 2016;633:279-289.
[73] Surdhar I, Gee M, Bouchard T, Coupland N, Malykhin N, Camicioli R. Intact limbic-prefrontal connections and reduced amygdala volumes in Parkinson's disease with mild depressive symptoms. Parkinsonism Relat Disord 2012;18:809-813.
[74] Huang P, Xu X, Gu Q, et al. Disrupted white matter integrity in depressed versus non-depressed Parkinson's disease patients: a tract-based spatial statistics study. J Neurol Sci 2014;346:145-148.
[75] Li W, Liu J, Skidmore F, Liu Y, Tian J, Li K. White matter microstructure changes in the thalamus in Parkinson disease with depression: A diffusion tensor MR imaging study. AJNR Am J Neuroradiol 2010;31:1861-1866.
[76] Salehi MA, Mohammadi S, Gouravani M, Javidi A, Dager SR. Brain microstructural alterations of depression in Parkinson's disease: A systematic review of diffusion tensor imaging studies. Hum Brain Mapp 2022;43:5658-5680.
[77] Hu X, Song X, Yuan Y, et al. Abnormal functional connectivity of the amygdala is associated with depression in Parkinson's disease. Mov Disord 2015;30:238-244.
[78] Lou Y, Huang P, Li D, et al. Altered brain network centrality in depressed Parkinson's disease patients. Mov Disord 2015;30:1777-1784.
[79] Carriere N, Besson P, Dujardin K, et al. Apathy in Parkinson's disease is associated with nucleus accumbens atrophy: a magnetic resonance imaging shape analysis. Mov Disord 2014;29:897-903.
[80] Alzahrani H, Antonini A, Venneri A. Apathy in Mild Parkinson's Disease: Neuropsychological and Neuroimaging Evidence. J Parkinsons Dis 2016;6:821-832.
[81] Theis H, Prange S, Bischof GN, et al. Impulsive-compulsive behaviour in early Parkinson's disease is determined by apathy and dopamine receptor D3 polymorphism. NPJ Parkinsons Dis 2023;9:154.
[82] Ge S, Liu J, Jia Y, Li Z, Wang J, Wang M. Topological alteration of the brain structural network in Parkinson's disease with apathy. Brain Res Bull 2024;208:110899.
[83] Baggio HC, Segura B, Garrido-Millan JL, et al. Resting-state frontostriatal functional connectivity in Parkinson's disease-related apathy. Mov Disord 2015;30:671-679.
[84] Lucas-Jimenez O, Ojeda N, Pena J, et al. Apathy and brain alterations in Parkinson's disease: a multimodal imaging study. Ann Clin Transl Neurol 2018;5:803-814.
[85] Robert G, Le Jeune F, Lozachmeur C, et al. Apathy in patients with Parkinson disease without dementia or depression: a PET study. Neurology 2012;79:1155-1160.
[86] Robert GH, Le Jeune F, Lozachmeur C, et al. Preoperative factors of apathy in subthalamic stimulated Parkinson disease: a PET study. Neurology 2014;83:1620-1626.
[87] Zoon TJC, Mathiopoulou V, van Rooijen G, et al. Apathy following deep brain stimulation in Parkinson's disease visualized by 7-Tesla MRI subthalamic network analysis. Brain Stimul 2023;16:1289-1291.
[88] Boon LI, Potters WV, Zoon TJC, et al. Structural and functional correlates of subthalamic deep brain stimulation-induced apathy in Parkinson's disease. Brain Stimul 2021;14:192-201.
[89] Prange S, Metereau E, Maillet A, et al. Limbic Serotonergic Plasticity Contributes to the Compensation of Apathy in Early Parkinson's Disease. Mov Disord 2022;37:1211-1221.
[90] Voon V, Napier TC, Frank MJ, et al. Impulse control disorders and levodopa-induced dyskinesias in Parkinson's disease: an update. Lancet Neurol 2017;16:238-250.
[91] Biundo R, Weis L, Facchini S, et al. Patterns of cortical thickness associated with impulse control disorders in Parkinson's disease. Mov Disord 2015;30:688-695.
[92] Cerasa A, Salsone M, Nigro S, et al. Cortical volume and folding abnormalities in Parkinson's disease patients with pathological gambling. Parkinsonism Relat Disord 2014;20:1209-1214.
[93] Pellicano C, Niccolini F, Wu K, et al. Morphometric changes in the reward system of Parkinson's disease patients with impulse control disorders. J Neurol 2015;262:2653-2661.
[94] Tessitore A, Santangelo G, De Micco R, et al. Cortical thickness changes in patients with Parkinson's disease and impulse control disorders. Parkinsonism Relat Disord 2016;24:119-125.
[95] Petersen K, Van Wouwe N, Stark A, et al. Ventral striatal network connectivity reflects reward learning and behavior in patients with Parkinson's disease. Hum Brain Mapp 2018;39:509-521.
[96] Carriere N, Lopes R, Defebvre L, Delmaire C, Dujardin K. Impaired corticostriatal connectivity in impulse control disorders in Parkinson disease. Neurology 2015;84:2116-2123.
[97] Maggi G, Loayza F, Vitale C, Santangelo G, Obeso I. Anatomical correlates of apathy and impulsivity co-occurrence in early Parkinson's disease. J Neurol 2024;271:2798-2809.
[98] Gescheidt T, Marecek R, Mikl M, et al. Functional anatomy of outcome evaluation during Iowa Gambling Task performance in patients with Parkinson's disease: an fMRI study. Neurol Sci 2013;34:2159-2166.
[99] Frosini D, Pesaresi I, Cosottini M, et al. Parkinson's disease and pathological gambling: results from a functional MRI study. Mov Disord 2010;25:2449-2453.
[100] van der Vegt JP, Hulme OJ, Zittel S, et al. Attenuated neural response to gamble outcomes in drug-naive patients with Parkinson's disease. Brain 2013;136:1192-1203.
[101] Tessitore A, De Micco R, Giordano A, et al. Intrinsic brain connectivity predicts impulse control disorders in patients with Parkinson's disease. Mov Disord 2017;32:1710-1719.
[102] Fenelon G, Alves G. Epidemiology of psychosis in Parkinson's disease. J Neurol Sci 2010;289:12-17.
[103] Carter R, Ffytche DH. On visual hallucinations and cortical networks: a trans-diagnostic review. J Neurol 2015;262:1780-1790.
[104] Lenka A, Jhunjhunwala KR, Saini J, Pal PK. Structural and functional neuroimaging in patients with Parkinson's disease and visual hallucinations: A critical review. Parkinsonism Relat Disord 2015;21:683-691.
[105] Ozawa M, Shiraishi T, Murakami H, et al. Structural MRI study of Pareidolia and Visual Hallucinations in Drug-Naive Parkinson's disease. Sci Rep 2024;14:31293.
[106] Bhome R, Thomas GEC, Zarkali A, Weil RS. Structural and Functional Imaging Correlates of Visual Hallucinations in Parkinson's Disease. Curr Neurol Neurosci Rep 2023;23:287-299.
[107] Watanabe H, Senda J, Kato S, et al. Cortical and subcortical brain atrophy in Parkinson's disease with visual hallucination. Mov Disord 2013;28:1732-1736.
[108] Pezzoli S, Cagnin A, Bandmann O, Venneri A. Structural and Functional Neuroimaging of Visual Hallucinations in Lewy Body Disease: A Systematic Literature Review. Brain Sci 2017;7.
[109] Yao N, Cheung C, Pang S, et al. Multimodal MRI of the hippocampus in Parkinson's disease with visual hallucinations. Brain Struct Funct 2016;221:287-300.
[110] Goetz CG, Vaughan CL, Goldman JG, Stebbins GT. I finally see what you see: Parkinson's disease visual hallucinations captured with functional neuroimaging. Mov Disord 2014;29:115-117.
[111] Yao N, Pang S, Cheung C, et al. Resting activity in visual and corticostriatal pathways in Parkinson's disease with hallucinations. Parkinsonism Relat Disord 2015;21:131-137.
[112] Yao N, Shek-Kwan Chang R, Cheung C, et al. The default mode network is disrupted in Parkinson's disease with visual hallucinations. Hum Brain Mapp 2014;35:5658-5666.
[113] Maillet A, Krack P, Lhommee E, et al. The prominent role of serotonergic degeneration in apathy, anxiety and depression in de novo Parkinson's disease. Brain 2016;139:2486-2502.
[114] Remy P, Doder M, Lees A, Turjanski N, Brooks D. Depression in Parkinson's disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain 2005;128:1314-1322.
[115] Prange S, Metereau E, Maillet A, et al. Early limbic microstructural alterations in apathy and depression in de novo Parkinson's disease. Mov Disord 2019;34:1644-1654.
[116] Vriend C, Pattij T, van der Werf YD, et al. Depression and impulse control disorders in Parkinson's disease: two sides of the same coin? Neurosci Biobehav Rev 2014;38:60-71.
[117] Lu Q, Zhu Z, Zhang H, et al. Shared and distinct cortical morphometric alterations in five neuropsychiatric symptoms of Parkinson's disease. Transl Psychiatry 2024;14:347.
Peer-review Terminology
Identity transparency: Single anonymized
Reviewer interacts with: Editor
Review information published:
Review reports
Reviewer identities if reviewer opts in
Author/reviewer communication
Details
© 2025 The Author(s). Brain Conflux published by Life Conflux Press Limited on behalf of Conflux Science.
This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
Publication History
Received 2025-01-19
Accepted 2025-03-18
Published 2025-03-30


